Irritable Bowel Syndrome
Irritable bowel syndrome is a functional gastrointestinal (GI) disorder, meaning symptoms are caused by changes in how the GI tract works. People with a functional GI disorder have frequent symptoms; however, the GI tract does not become damaged. IBS is a group of symptoms that occur together, not a disease. In the past, IBS was called colitis, mucous colitis, spastic colon, nervous colon, and spastic bowel. The name was changed to reflect the understanding that the disorder has both physical and mental causes and is not a product of a person’s imagination.
IBS is diagnosed when a person has had abdominal pain or discomfort at least three times a month for the last 3 months without other disease or injury that could explain the pain. The pain or discomfort of IBS may occur with a change in stool frequency or consistency or be relieved by a bowel movement.
IBS is often classified into four subtypes based on a person’s usual stool consistency. These subtypes are important because they affect the types of treatment that are most likely to improve the person’s symptoms. The four subtypes of IBS are
- IBS with constipation (IBS-C)
- hard or lumpy stools at least 25 percent of the time
- loose or watery stools less than 25 percent of the time
- IBS with diarrhea (IBS-D)
- loose or watery stools at least 25 percent of the time
- hard or lumpy stools less than 25 percent of the time
- Mixed IBS (IBS-M)
- hard or lumpy stools at least 25 percent of the time
- loose or watery stools at least 25 percent of the time
- Unsubtyped IBS (IBS-U)
- hard or lumpy stools less than 25 percent of the time
- loose or watery stools less than 25 percent of the time
What is the GI tract?
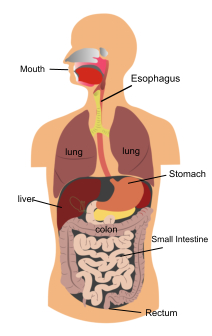 The organs of the GI tract
The organs of the GI tractThe GI tract is a series of hollow organs joined in a long, twisting tube from the mouth to the anus—the opening through which stool leaves the body. Food is digested by the movement of muscles in the GI tract, along with the release of hormones and enzymes. Organs that make up the GI tract are the mouth, esophagus, stomach, small intestine, large intestine—which includes the appendix, cecum, colon, and rectum—and anus. The intestines are sometimes called the bowel. The last part of the GI tract—called the lower GI tract—consists of the large intestine and anus.
The large intestine absorbs water and any remaining nutrients from partially digested food passed from the small intestine. The large intestine then changes waste from liquid to a solid matter called stool. Stool passes from the colon to the rectum. The rectum is located between the last part of the colon—called the sigmoid colon—and the anus. The rectum stores stool prior to a bowel movement. During a bowel movement, stool moves from the rectum to the anus.
What are the symptoms of IBS?
The most common symptoms of IBS are abdominal pain or discomfort, often reported as cramping, along with changes in bowel habits. To meet the definition of IBS, the pain or discomfort will be associated with at least two of the following three symptoms:
- bowel movements that occur more or less often than usual
- stool that appears less solid and more watery, or harder and more lumpy, than usual
- bowel movements that improve the discomfort
Other symptoms of IBS may include
- diarrhea—having loose, watery stools three or more times a day and feeling urgency to have a bowel movement.
- constipation—having fewer than three bowel movements a week. During a bowel movement, stools can be hard, dry, and small, making them difficult to pass. Some people find it painful and often have to strain to have a bowel movement.
- feeling that a bowel movement is incomplete.
- passing mucus—a clear liquid made by the intestines that coats and protects tissues in the GI tract.
- abdominal bloating.
What causes IBS?
The causes of IBS are not well understood. Researchers believe a combination of physical and mental health problems can lead to IBS.
Brain-Gut Signal Problems
Signals between the brain and nerves of the small and large intestines, also called the gut, control how the intestines work. Problems with brain-gut signals may cause IBS symptoms, such as changes in bowel habits and pain or discomfort.
GI Motor Problems
Normal motility, or movement, may not be present in the colon of a person who has IBS. Slow motility can lead to constipation and fast motility can lead to diarrhea. Spasms, or sudden, strong muscle contractions that come and go, can cause abdominal pain. Some people with IBS also experience hyperreactivity—a dramatic increase in bowel contractions in response to stress or eating.
Hypersensitivity
People with IBS have a lower pain threshold for bowel stretching caused by gas or stool compared with people who do not have IBS. The brain may process pain signals from the bowel differently in people with IBS.
Mental Health Problems
Mental health, or psychological, problems such as panic disorder, anxiety, depression, and post-traumatic stress disorder are common in people with IBS. The link between these disorders and development of IBS is unclear. GI disorders, including IBS, are often found in people who have reported past physical or sexual abuse. Researchers believe people who have been abused tend to express psychological stress through physical symptoms.
Bacterial Gastroenteritis
Some people who have bacterial gastroenteritis—an infection or irritation of the stomach and intestines caused by bacteria—develop IBS. Researchers do not know why gastroenteritis leads to IBS in some people and not others, though abnormalities of the GI tract lining and psychological problems may be factors.
Small Intestinal Bacterial Overgrowth
Normally, few bacteria live in the small intestine. Small intestinal bacterial overgrowth is an increase in the number or a change in the type of bacteria in the small intestine. These bacteria can produce extra gas and may also cause diarrhea and weight loss. Some researchers believe that small intestinal bacterial overgrowth may lead to IBS, and some studies have shown antibiotics to be effective in treating IBS. However, more research is needed to show a link between small intestinal bacterial overgrowth and IBS.
Body Chemicals
People with IBS have altered levels of neurotransmitters—chemicals in the body that transmit nerve signals—and GI hormones, though the role these chemicals play in developing IBS is unclear. Younger women with IBS often have more symptoms during their menstrual periods. Post-menopausal women have fewer symptoms compared with women who are still menstruating. These findings suggest that reproductive hormones can worsen IBS problems.
Genetics
Whether IBS has a genetic cause, meaning it runs in families, is unclear. Studies have shown IBS is more common in people with family members who have a history of GI problems. However, the cause could be environmental or the result of heightened awareness of GI symptoms.
Food Sensitivity
Many people with IBS report that symptoms are triggered by foods rich in carbohydrates, spicy or fatty foods, coffee, and alcohol. However, people with food sensitivity typically do not have clinical signs of food allergy. Researchers have proposed that symptoms may result from poor absorption of sugars or bile acids, which help break down fats and get rid of wastes in the body.
How is IBS treated?
Though IBS does not have a cure, the symptoms can be treated with a combination of
- changes in eating, diet, and nutrition
- medications
- probiotics
- therapies for mental health problems
Eating, Diet, and Nutrition
Large meals can cause cramping and diarrhea, so eating smaller meals more often, or eating smaller portions, may help IBS symptoms. Eating meals that are low in fat and high in carbohydrates, such as pasta, rice, whole-grain breads and cereals, fruits, and vegetables, may help.
Certain foods and drinks may cause IBS symptoms in some people, such as
- foods high in fat
- some milk products
- drinks with alcohol or caffeine
- drinks with large amounts of artificial sweeteners, which are used in place of sugar
- beans, cabbage, and other foods that may cause gas
People with IBS may want to limit or avoid these foods. Keeping a food diary is a good way to track which foods cause symptoms so they can be excluded from or reduced in the diet.
Dietary fiber may improve constipation symptoms in people with IBS, although it may not help with reducing pain. Fiber softens stool so it moves smoothly through the colon. Adults are advised to consume 21 to 38 grams of fiber a day.3 Fiber may cause gas and trigger symptoms in some people with IBS. Increasing fiber intake slowly, by 2 to 3 grams a day, may help reduce the risk of increased gas and bloating.
Medications
A health care provider will select medications based on a person’s symptoms.
- Fiber supplements may be recommended to relieve constipation when increasing dietary fiber is ineffective.
- Laxatives may help constipation. Laxatives work in different ways, and a health care provider can provide information about which type is best for each person. Read more in Constipation at www.digestive.niddk.nih.gov.
- Loperamide is an antidiarrheal that has been found to reduce diarrhea in people with IBS, though it does not reduce pain, bloating, or other symptoms. Loperamide reduces stool frequency and improves stool consistency by slowing the movement of stool through the colon.
- Antispasmodics, such as hyoscine, cimetropium, and pinaverium, help to control colon muscle spasms and reduce abdominal pain.
- Antidepressants, such as low doses of tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs), can help relieve IBS symptoms, including abdominal pain. In theory, TCAs should be better for people with IBS-D and SSRIs should be better for people with IBS-C due to the effect on colon transit, although this theory has not been confirmed in clinical studies. TCAs work in people with IBS by reducing sensitivity to pain in the GI tract as well as normalizing GI motility and secretion.
- Lubiprostone (Amitiza) is prescribed for people who have IBS-C. The medication has been found to improve abdominal pain or discomfort, stool consistency, straining, and constipation severity.
- Linaclotide (Linzess) is also prescribed for people who have IBS-C. Linzess has been found to relieve abdominal pain and increase the frequency of bowel movements.
The antibiotic rifaximin can reduce abdominal bloating by treating small intestinal bacterial overgrowth; however, scientists are still debating the use of antibiotics to treat IBS and more research is needed.
Probiotics
Probiotics are live microorganisms, usually bacteria, that are similar to microorganisms normally found in the GI tract. Studies have found that when taken in large enough amounts, probiotics, specifically Bifidobacteria and certain probiotic combinations, improve symptoms of IBS. However, more research is needed. Probiotics can be found in dietary supplements, such as capsules, tablets, and powders, and in some foods, such as yogurt. A health care provider can give information about the right kind and amount of probiotics to take to improve IBS symptoms. To help ensure coordinated and safe care, people should discuss their use of complementary and alternative medical practices, including their use of dietary supplements and probiotics, with their health care provider. Read more at www.nccam.nih.gov/health/probiotics.
Therapies for Mental Health Problems
The following therapies can help improve IBS symptoms due to mental health problems:
- Talk therapy may reduce stress and improve IBS symptoms. Two types of talk therapy used to treat IBS are cognitive behavioral therapy and psychodynamic, or interpersonal, therapy. Cognitive behavioral therapy focuses on a person’s thoughts and actions. Psychodynamic therapy focuses on how emotions affect IBS symptoms. This type of therapy often involves relaxation and stress management techniques.
- Hypnotherapy may help a person relax the muscles in the colon.
- Mindfulness training teaches people to focus their attention on sensations occurring at the moment and avoid catastrophizing, or worrying about the meaning of those sensations.
3- Dietary reference intakes: recommended dietary allowances and adequate intakes, total water and macronutrients. In: Ross AC, Taylor CL, Yaktine AL, Del Valle HB, eds. Dietary Reference Intakes for Calcium and Vitamin D. Washington, D.C.: The National Academies Press; 2011: 1110.
Symptoms may often occur after eating a meal. To meet the definition of IBS, symptoms must occur at least three times a month.
If you have any questions or wish to schedule an appointment, please do not hesitate to call the office at (706) 548-0058. Remember that we usually require that you see a primary care physician (your family doctor or PCP) before we can schedule you. If you are having a medical emergency, get medical attention immediately at your nearest healthcare provider:
Athens Regional Medical Center: (706) 475-7000
St. Mary's Hospital: (706) 354-3000
This informational material is taken from the National Digestive Diseases Information Clearinghouse, a division of the U.S. Department of Health and Human Resources.
Please see the Contact Us page for street maps.
Click here to
Request an Appointment.